03 Feb 2026
Rhinoplasty Revision Surgery in Mohali: Cost When Your First Nose Job Fails

Dr. Puneet Kumar
30 Oct 2025
Call +91 80788 80788 to request an appointment.
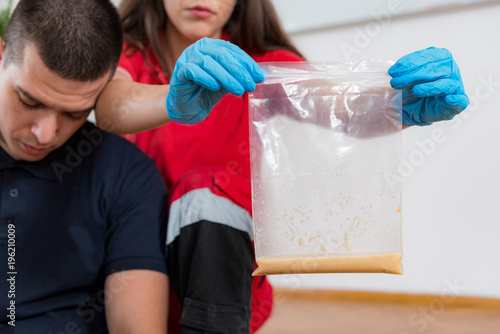
Livasa Hospitals — serving communities across Punjab including Livasa Mohali, Livasa Amritsar, Livasa Hoshiarpur and Livasa Khanna — provides 24/7 emergency toxicology and poisoning care. If you are facing a suspected poisoning emergency, call us immediately at +91 80788 80788 or visit Book an appointment / emergency help.
Poisoning emergencies can be sudden, frightening, and life-threatening. They include accidental exposures to household chemicals, industrial chemical incidents, medication overdoses (intentional or accidental), bites and envenomations, and exposure to environmental toxins. In a diverse state such as Punjab — where agricultural chemicals, industrial solvents and widespread availability of medicines co-exist — rapid recognition and timely care are essential to reduce morbidity and mortality. This guide is designed to help patients, families, first responders and caregivers understand what to do when someone is poisoned, what to expect at the emergency department, and how Livasa Hospitals in Mohali, Amritsar, Hoshiarpur and Khanna deliver emergency toxicology and poisoning treatment in Punjab.
This article covers common causes of poisoning in our region, the typical symptoms to watch for, immediate first-aid measures, diagnostic and treatment options available at Livasa Hospitals, pediatric considerations, prevention strategies, local resources including poison control Punjab contacts, and practical information about access and costs. It is written in a patient-friendly, authoritative style and uses current emergency-care principles. When in doubt, always prioritize calling emergency services or Livasa Hospitals emergency line at +91 80788 80788.
A poisoning emergency occurs when a person is exposed to a substance that causes harmful physiological effects rapidly or is likely to do so if untreated. Causes range from ingestion of medicines, pesticides, and household cleaners to inhalation of gases and dermal exposure to corrosive or toxic substances. Poisoning emergencies are not limited to adults — children and older adults are particularly vulnerable due to differences in size, metabolism, intentionality and comorbidities. In Punjab, agricultural pesticide exposure and pharmaceutical overdoses are common reasons for emergency toxicology referrals.
Clinically, an emergency is defined not only by the presence of a toxic substance but by the severity and progression of symptoms: respiratory compromise, altered consciousness, seizures, arrhythmias, hypotension, metabolic abnormalities (acidosis, hypoglycemia) and multi-organ dysfunction. Many poisons act quickly and may cause irreversible harm when treatment is delayed. For this reason, time is critical: early assessment at an emergency toxicology unit such as those at Livasa Mohali and Livasa Amritsar can mean the difference between full recovery and severe complications.
Emergency departments offering poison care must be equipped to provide rapid stabilization (airway, breathing, circulation), laboratory evaluation, specific antidotes, decontamination (when appropriate), advanced supportive care including ventilatory support and dialysis when required. Our teams in Mohali, Amritsar, Hoshiarpur and Khanna follow standardized emergency toxicology protocols and maintain 24/7 availability to manage acute poisoning efficiently.
Patterns of poisoning reflect local industry, lifestyle and seasonal activities. In Punjab, the following exposures are commonly seen in emergency departments:
In addition to the agent, risk factors that increase severity include delayed presentation, large dose, young age, co-existing medical illnesses, and lack of immediate decontamination. Livasa Hospitals’ emergency toxicology services in Punjab focus on rapid identification of the type of exposure, considering local patterns (pesticide seasonality during sowing/harvest), and initiating evidence-based treatment pathways.
Symptoms of poisoning vary greatly by toxin, route (ingestion, inhalation, dermal), dose and time since exposure. However, certain clinical features suggest a poisoning emergency and should prompt immediate medical attention. Look for:
For parents and caregivers, watch children for sudden behavioral change, unexplained vomiting, drowsiness or burns around the mouth. Always bring the container, label, or a photograph of the substance to the emergency department if possible; this accelerates identification and selection of appropriate antidote therapies at Livasa emergency toxicology centers across Punjab.
Immediate action can reduce harm. The priorities are to keep the patient safe, avoid further exposure, and get them to a facility promptly. Follow these steps:
These measures are intended to stabilize and limit harm before arrival at a facility. When you call Livasa Hospitals in Punjab, our triage team can advise on immediate interventions and prepare the emergency toxicology team to receive the patient.
On arrival at any Livasa emergency facility (Mohali, Amritsar, Hoshiarpur, Khanna), the team follows a structured approach: immediate stabilization (airway, breathing, circulation), triage of vital signs, targeted history-taking, and rapid diagnostics. Our emergency departments are equipped with point-of-care testing, imaging and access to specialty labs for toxin identification when needed.
Typical evaluation steps include:
Rapid diagnostics at Livasa Hospitals help clinicians determine whether decontamination, antidote administration, supportive care or extracorporeal removal is required. Our emergency toxicology teams are trained to interpret results in the context of local poisoning patterns in Punjab.
Treatment depends on the poison, severity, and time since exposure. Interventions used by Livasa Hospitals’ emergency toxicology teams include general supportive care, decontamination, specific antidotes, enhanced elimination techniques and critical care support. Below are commonly used modalities, along with indications:
The choice between methods depends on the toxicity profile. The table below compares common treatment approaches to help patients understand the differences and expected indications.
| Treatment modality | Benefits | When used |
|---|---|---|
| Supportive care | Stabilizes vital functions; first-line for most poisonings | All emergencies |
| Activated charcoal | Binds many oral toxins and reduces absorption | Select oral ingestions within time window |
| Antidotes (e.g., naloxone, NAC) | Directly counteracts toxin effects; can be lifesaving | When specific toxin identified or strongly suspected |
| Hemodialysis/hemoperfusion | Removes dialyzable toxins and corrects metabolic disturbances | Severe poisoning with dialyzable substances |
Livasa Hospitals maintains rapid access to antidotes and dialysis services in Mohali and Amritsar, and can coordinate transfers from Hoshiarpur and Khanna for patients requiring advanced extracorporeal therapies.
Children, pregnant women, older adults and patients with chronic illnesses require special attention. In Punjab, household exposures and accidental ingestions account for a large proportion of pediatric poisonings. Children have smaller body mass and may become severely affected by relatively small amounts of toxic substances. Signs such as lethargy, persistent vomiting, seizures or unusual drooling in a child warrant immediate evaluation.
Key pediatric considerations:
Livasa Hospitals pediatric emergency teams are trained in age-appropriate resuscitation and dosing, and pediatric-specific protocols are in place to ensure rapid, safe treatment. For families in Punjab, immediate presentation to a Livasa emergency center or contacting the emergency line may allow early treatments that substantially improve outcomes.
Prevention is the most effective strategy to reduce poisoning incidents. In Punjab, community-level interventions focused on safer pesticide storage, education on drug safety, and childproofing homes can mitigate risk. Livasa Hospitals partners with local public health initiatives and provides educational materials to families, schools and workplaces.
Practical prevention tips:
Community resources in Punjab:
If you are a community leader or employer in Punjab and would like prevention workshops or collaborative programs, contact Livasa Hospitals at +91 80788 80788.
The cost of poisoning treatment in Punjab varies with severity, need for ICU care, antidotes, duration of hospitalization and the requirement for procedures such as hemodialysis. Below is a general comparison to help families plan financially while emphasizing that immediate care should never be delayed due to cost concerns — early treatment often reduces total expense by preventing complications.
| Treatment category | Typical cost range (approx.) | Notes |
|---|---|---|
| Minor outpatient care | ₹2,000 – ₹15,000 | For observation, activated charcoal, brief monitoring |
| Inpatient non-ICU | ₹15,000 – ₹80,000 | Includes antidotes and lab tests |
| ICU care with antidotes | ₹80,000 – ₹300,000+ | Mechanical ventilation, vasopressors, extended monitoring |
| Extracorporeal removal (dialysis) | ₹20,000 – ₹200,000+ | Depends on sessions and ICU stay |
These are approximate ranges; actual costs depend on hospital policies, duration of stay and individual patient needs. Livasa Hospitals offers an upfront financial counselling service in Mohali and Amritsar to help families understand expected bills and explore available assistance. For specialized cases, such as severe industrial chemical exposures that require long-term rehabilitation, early referral to tertiary centers is arranged and coordinated by the Livasa network across Punjab.
When to seek specialized care:
Understanding differences among common poisoning scenarios helps patients and families appreciate urgency and expected treatments. Below is a concise comparison presented in table form for clarity.
| Poisoning type | Typical presentation | Immediate response |
|---|---|---|
| Household chemical | Burns, drooling, vomiting, breathing difficulty | Irrigate skin/eyes, don’t induce vomiting for caustics, seek ED |
| Industrial chemical | Fumes, multi-worker exposure, severe respiratory or neurologic signs | Move to fresh air, decontaminate, call emergency services and Livasa |
| Drug overdose | Altered consciousness, respiratory depression (opioids), agitation | Support airway, give antidote if available (e.g., naloxone), urgent ED |
Poisoning remains a significant public health problem globally and locally. The World Health Organization estimates that tens of thousands of deaths each year are attributable to unintentional poisonings worldwide, while intentional self-poisoning contributes substantially to global suicide statistics. In India, pesticide-related poisonings, especially in rural agricultural communities, are an important contributor to poison-related mortality. In Punjab, seasonal increases in pesticide exposures and workplace-related industrial chemical incidents create predictable local surges in emergency admissions.
At Livasa Hospitals, our emergency departments monitor poisoning trends across Mohali, Amritsar, Hoshiarpur and Khanna to ensure adequate staffing, supplies of antidotes and readiness for seasonal peaks. Although exact figures vary year to year, data-driven public health responses — including targeted education for farmers about safe pesticide storage, and community programs to reduce access to harmful agents — have measurable impacts in reducing both accidental and intentional poisoning rates.
For up-to-date local statistics or collaborative public health initiatives, contact Livasa Hospitals’ community outreach team via our booking page or call +91 80788 80788.
If you suspect poisoning, call emergency services and Livasa Hospitals immediately. Use +91 80788 80788 to reach our emergency triage. When contacting us, be prepared to provide:
Livasa Hospitals provides:
Follow-up care is arranged before discharge and can include psychiatric counselling, occupational health assessments for workplace exposures, and coordination with public health for community prevention measures. Use our website https://www.livasahospitals.com/appointment to book non-emergency consultations or to get guidance from our specialists.
If you suspect a poisoning emergency in Punjab, do not wait. Call +91 80788 80788 now to reach Livasa Hospitals emergency triage. For faster intake, bring any containers or photos of the substance and proceed to the nearest Livasa centre: Livasa Mohali, Livasa Amritsar, Livasa Hoshiarpur or Livasa Khanna. You can also book emergency assistance online. Early care saves lives.
Disclaimer: This guide provides general information and does not replace professional medical advice. In any suspected poisoning, prioritize calling emergency services or the Livasa Hospitals emergency number. Statistics and costs are approximate and intended to provide context; actual care decisions are individualized by clinicians at Livasa Hospitals.
Rhinoplasty Revision Surgery in Mohali: Cost When Your First Nose Job Fails
Plastic Surgery After Massive Weight Loss: Body Contouring Packages in Mohali
ENT + Cosmetic in Mohali: Septoplasty for Breathing with Cosmetic Rhinoplasty Offers
Livasa Healthcare Group Corporate Office,Phase-8, Industrial Area, Sector 73, Sahibzada Ajit Singh Nagar, Punjab 160071
| Mohali | +91-99888 23456 |
| Amritsar | +91-99887 49494 |
| Hoshiarpur | +91-99883 35353 |
| Nawanshahr | +91-75081 82337 |
| Khanna | +91-98888 05394 |