03 Feb 2026
Rhinoplasty Revision Surgery in Mohali: Cost When Your First Nose Job Fails

Dr. Amanjot Singh
17 Nov 2025
Call +91 80788 80788 to request an appointment.
Livasa Hospitals, Livasa Amritsar provides comprehensive care for patients with intracerebral hemorrhage (ICH) and associated bleeding disorders in Amritsar and the surrounding regions of Punjab. This article explains what an intracerebral hemorrhage is, how bleeding disorders influence risk and management, the full spectrum of diagnosis and treatment options available locally, and how timely care at a neurology hospital in Amritsar can improve outcomes. If you or a loved one are concerned about signs of brain bleed, call us at +91 80788 80788 or book an appointment online at Livasa Hospitals.
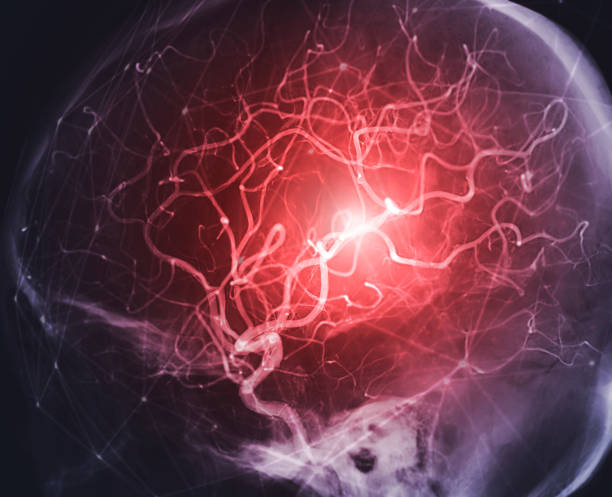
Intracerebral hemorrhage (ICH), commonly called a brain bleed, occurs when a blood vessel within the brain ruptures and bleeds into the surrounding brain tissue. This causes mechanical damage from the expanding hematoma and secondary injury from increased intracranial pressure, local ischemia, and inflammatory responses. ICH is a subtype of hemorrhagic stroke and accounts for approximately 10–15% of all strokes worldwide but contributes disproportionately to mortality and severe disability.
In India and in Punjab specifically, burden of ICH remains high due to uncontrolled hypertension, growing use of anticoagulant medications, and constraints in early emergency response. Local centers such as Livasa Amritsar have developed integrated neurology and neurosurgery teams to provide rapid imaging, anticoagulation reversal, surgical care, and post-acute rehabilitation to reduce long-term disability. Recognizing ICH early and acting quickly is the single most important factor in preventing life-threatening complications.
This guide is written for patients, families, and community members in Amritsar and Punjab to explain causes, symptoms, diagnostic steps, emergency care pathways, treatment alternatives, expected outcomes, and prevention strategies. It emphasizes the interplay between primary bleeding disorders (like hemophilia) and acquired coagulation problems (such as anticoagulant therapy or liver disease), and how each situation is managed differently at specialized centres like Livasa Hospitals.
Intracerebral hemorrhage results from rupture of small intracerebral arteries and arterioles. The most important global cause is chronic, uncontrolled hypertension which damages small vessel walls leading to microaneurysms that can rupture. In addition to hypertension, other causes and risk factors include:
In Amritsar and surrounding districts in Punjab, major contributors to ICH are similar to national patterns: poorly controlled hypertension, rising anticoagulant use in an aging population, and limited early recognition of bleeding symptoms. Epidemiological data show that stroke incidence in India is increasing; hemorrhagic strokes represent a larger proportion of strokes in South Asia than in many high-income countries. Estimates suggest ICH mortality within the first 30 days can exceed 30–40% globally, and outcomes are worse without rapid access to specialist care. These statistics underline the importance of adequate blood-pressure control, careful anticoagulant management, and access to specialized bleeding disorder clinics in Punjab.
Symptoms of intracerebral hemorrhage can vary depending on the site and size of the bleed. Sudden onset is common — patients frequently report a rapid progression of symptoms over minutes to hours. Recognizing early warning signs is vital because immediate evaluation and treatment at a neurology hospital in Amritsar can be lifesaving.
Common presenting features include:
For individuals with known bleeding disorders or on anticoagulation in Amritsar, even milder symptoms (such as new mild weakness or transient confusion) require urgent assessment for intracranial bleeding because smaller hematomas may expand rapidly. Local search terms like “signs of brain bleed Amritsar” and “intracerebral hemorrhage symptoms Amritsar” are important to know: if any sudden neurological change occurs, call emergency services or present directly to the nearest stroke-capable center such as Livasa Amritsar.
Time is critical. Early presentation allows for CT imaging, reversal of anticoagulation, and appropriate monitoring or surgical management. Delayed care increases the risk of hematoma expansion and secondary brain injury, leading to worse functional outcomes.
Rapid and accurate diagnosis distinguishes hemorrhagic stroke from ischemic stroke and determines the correct treatment pathway. At Livasa Hospitals in Amritsar, an emergency neurology and radiology team aims to perform essential investigations immediately upon arrival.
Key diagnostic steps include:
In the context of anticoagulation, timely laboratory data enable targeted reversal strategies. For example, an elevated INR in a warfarin-treated patient mandates prompt administration of vitamin K and prothrombin complex concentrate (PCC) or fresh frozen plasma according to protocols. Similarly, suspected DOAC-associated bleeding may be managed with specific reversal agents when available.
At Livasa Amritsar, coordinated workflows prioritize rapid imaging and laboratory turnaround. Tele-neurology consultations and stroke team activation can streamline transfer or in-hospital escalation. Accurate early diagnosis also informs the need for neurosurgical referral, intensive care monitoring, and initiation of rehabilitation planning.
Management of intracerebral hemorrhage combines immediate stabilisation, specific interventions to limit hematoma expansion, and decisions about surgical evacuation when indicated. The choice between conservative and surgical treatment depends on hematoma size, location, neurological status, patient's premorbid condition, and presence of increased intracranial pressure.
Initial medical management objectives include airway protection, blood pressure control, reversal of coagulopathy, seizure prevention, and intracranial pressure management. Blood pressure lowering in the acute phase is a cornerstone — target systolic blood pressure is individualized but many protocols aim for <140–160 mmHg depending on patient factors and SBP at presentation. Antipyretic and glycemic control also reduce secondary injury.
Specific interventions:
Surgical strategies include open craniotomy, minimally invasive catheter-based hematoma aspiration, endoscopic evacuation, and stereotactic aspiration. The choice depends on clot size, location, and patient stability. Minimally invasive approaches can decrease operative trauma and improve recovery times, while open surgical evacuation may be necessary for large or complicated bleeds.
| Procedure type | Benefits | Recovery time |
|---|---|---|
| Minimally invasive (catheter/aspiration) | Smaller incision, reduced tissue trauma, lower infection risk | Several days to 2 weeks |
| Endoscopic evacuation | Direct visualization, targeted clot removal, less blood loss | 1–2 weeks |
| Open craniotomy | Comprehensive access for large or complex bleeds | 2–6 weeks or longer |
At Livasa Amritsar, multidisciplinary discussions between neurologists, neurosurgeons, critical care specialists, and hematologists inform individualized decisions. For patients with concurrent bleeding disorders, hematology input is essential before any operative plan. Timely and targeted reversal of coagulopathy can make surgical options safer and conserve neurological function.
When intracerebral hemorrhage occurs in a patient with a known bleeding disorder or who is taking anticoagulants, management must address both the intracranial bleed and the underlying hemostatic abnormality. Treatment differs significantly between congenital bleeding disorders (hemophilia, von Willebrand disease) and acquired coagulopathies (warfarin, DOACs, liver disease, DIC).
Key management principles include rapid correction of the coagulation defect, targeted transfusion strategies, and specialist hematology involvement. For congenital factor deficiencies, specific factor concentrates (factor VIII, IX) are preferred, and desmopressin (DDAVP) can be useful for some patients with mild hemophilia A or certain types of von Willebrand disease. For thrombocytopenia or platelet dysfunction from drugs, platelet transfusion may be required.
Below is a practical comparison of common reversal agents and interventions used in ICH associated with anticoagulation or bleeding disorders:
| Cause | Preferred reversal | Notes |
|---|---|---|
| Warfarin (elevated INR) | Prothrombin complex concentrate (PCC) + IV vitamin K | PCC provides rapid factor restoration; FFP if PCC unavailable. |
| Dabigatran | Idarucizumab (specific antidote) | Rapid and specific reversal; dialysis option for dabigatran if necessary. |
| Factor Xa inhibitors (apixaban, rivaroxaban) | Andexanet alfa (if available) or PCC | Andexanet provides targeted reversal; PCC used when unavailable. |
| Hemophilia A or B | Factor VIII or IX concentrates; bypassing agents if inhibitors present | Specialist hematology care required; dosing individualized. |
| Thrombocytopenia or antiplatelet effect | Platelet transfusion; desmopressin in certain cases | Evaluate risks and benefits carefully; platelet function tests helpful. |
In Punjab, availability of specific reversal agents such as andexanet alfa may be limited; therefore, hospitals like Livasa Amritsar maintain established protocols using PCC, idarucizumab, and readily available blood products while liaising with specialized supply chains to secure antidotes when possible. Hematology consultation and close ICU monitoring are crucial in these complex scenarios to balance bleeding control against thrombotic risks that may arise after reversal.
Recovery after intracerebral hemorrhage is variable and depends on the size and location of the bleed, speed of initial management, patient age, premorbid health, and presence of coexisting conditions. Immediate mortality for ICH is high, but many survivors can improve significantly with multidisciplinary rehabilitation.
Rehabilitation focuses on maximizing functional independence and reducing complications such as contractures, aspiration pneumonia, and depression. Key components include:
Prognosis: Functional outcomes are often described using scales such as the modified Rankin Scale (mRS). Many patients with moderate ICH will have residual disability but can regain substantial independence with early and intensive rehabilitation. Long-term mortality remains elevated compared to ischemic stroke. Local data from tertiary centers in India indicate that specialized stroke units and rehabilitation services substantially improve outcomes and reduce length of hospital stay. Livasa Amritsar supports coordinated transition from acute care to rehabilitation, working with physiotherapists, speech therapists, and vocational counsellors to facilitate reintegration into daily life.
Regular follow-up within stroke clinics is essential, with periodic imaging, blood pressure monitoring, and medication adjustment. For patients with underlying bleeding disorders, ongoing hematology follow-up and plans for safe future anticoagulant use (if needed) must be personalized.
Cost considerations for intracerebral hemorrhage treatment vary depending on the need for ICU care, imaging, blood products, reversal agents, and surgical procedures. In Amritsar and Punjab, cost differences can also reflect the type of facility, availability of specialized neurosurgical teams, and length of stay. Below is a general comparison to help patients and families understand potential ranges; actual costs should be confirmed with Livasa Amritsar billing for tailored estimates.
| Service | Typical cost range (Amritsar, INR) | Notes |
|---|---|---|
| Emergency CT brain | 2,500–7,000 | Urgent imaging price varies by center and need for contrast/CTA. |
| ICU per day | 10,000–40,000 | Dependent on level of monitoring and ventilator support. |
| PCC dose (for reversal) | 30,000–80,000 | High variation by product and dose required. |
| Surgical evacuation | 70,000–300,000 | Range reflects type of surgery, implants, ICU duration. |
| Rehabilitation per week | 5,000–25,000 | Depends on intensity and facility. |
These estimates are illustrative; Livasa Hospitals offers transparent billing and can provide pre-admission cost counselling for families. When choosing a hospital for brain hemorrhage in Amritsar or Punjab, consider:
Livasa Amritsar aims to provide all these services with prompt coordination, compassionate care, and options for financial counselling and insurance facilitation.
If someone in Amritsar or nearby develops sudden neurological symptoms — severe headache, weakness, speech difficulty, sudden confusion, loss of balance, or seizures — seek emergency care without delay. For patients with known bleeding disorders, any new head injury or neurological change warrants immediate assessment even if initial symptoms seem mild.
Local resources and steps:
Livasa Amritsar provides an integrated team that includes neurology, neurosurgery, hematology, critical care, radiology, and physiotherapy to offer rapid, coordinated care. Nearby neighborhoods and locations served include the greater Amritsar city catchment and surrounding districts across central Punjab, ensuring patients can access emergency brain bleed treatment in Amritsar when needed.
Preventing intracerebral hemorrhage focuses on controlling modifiable risks and educating patients with bleeding disorders or on anticoagulation. Practical prevention measures relevant to Amritsar and Punjab include:
Follow-up after any ICH should be structured: early post-discharge clinic visits, repeat imaging when indicated, blood pressure and medication reviews, and rehabilitation plans. For patients in Amritsar, Livasa Hospitals offers follow-up clinics combining neurology and hematology input to optimize secondary prevention and reduce recurrence risk. Community awareness programs and patient education on signs of brain bleed and safe medication use can lower delays in seeking care and improve outcomes across Punjab.
Finally, for families searching online, common local search phrases such as “brain hemorrhage Amritsar,” “ICH treatment Amritsar,” “bleeding disorders Punjab,” and “best neurosurgeon Amritsar” should lead you to stroke-capable centres like Livasa Amritsar that provide rapid imaging, anticoagulation reversal, surgical options, and comprehensive rehabilitation.
If you are experiencing symptoms suggestive of a brain bleed, do not wait. Call Livasa Amritsar at +91 80788 80788 or book an emergency appointment online. Our multidisciplinary stroke and coagulation team provides evidence-based intracerebral hemorrhage treatment in Punjab, including rapid anticoagulation reversal, sophisticated imaging, neurosurgical interventions, and rehabilitation services tailored to each patient.
Livasa Hospitals is committed to compassionate, patient-centered care for hemorrhagic stroke, bleeding disorders, and complex coagulation problems in Amritsar and across Punjab. Early presentation and specialist management save lives and improve recovery—reach out now for immediate support.
Disclaimer: This article provides general information and is not a substitute for professional medical advice. Individual cases vary and care decisions should be made with your treating team. For personalized guidance, contact Livasa Hospitals, Livasa Amritsar at +91 80788 80788 or visit https://www.livasahospitals.com/appointment.
Rhinoplasty Revision Surgery in Mohali: Cost When Your First Nose Job Fails
Plastic Surgery After Massive Weight Loss: Body Contouring Packages in Mohali
ENT + Cosmetic in Mohali: Septoplasty for Breathing with Cosmetic Rhinoplasty Offers
Livasa Healthcare Group Corporate Office,Phase-8, Industrial Area, Sector 73, Sahibzada Ajit Singh Nagar, Punjab 160071
| Mohali | +91-99888 23456 |
| Amritsar | +91-99887 49494 |
| Hoshiarpur | +91-99883 35353 |
| Nawanshahr | +91-75081 82337 |
| Khanna | +91-98888 05394 |